The expression ‘centric interference’ is difficult for dentists to understand because centric is a TMJ term and interference is a tooth term. The anterior control is the first force point to touch and often is a diagnostic tool in finding the dominant controlling centric interference.
- Anterior in ‘anterior guidance’ means “in front of the condyles.”
- The first tooth to contact when the condyles are braced is called your ‘anterior control.’
- The ‘anterior control’ is the start of your CR to CO slide (also known as your centric to MIP slide).
- Most occlusions have an ‘anterior control’ on a posterior tooth.
Dr. George Hollenbeck said: “They make too much of this. Occlusion is just a good centric, and no interferences, and the rest is all hogwash. The basics are simple; it is the involvement and refinements of accomplishing those objectives that become complicated. The mastery of these concepts never ceases in ones career.”
“No interferences” is synonymous with “good anterior guidance.” In order to understand the difference between good and bad anterior guidance, we must define the words “anterior” and “guidance” separately. The word “anterior” is an adjective meaning “near the front.” In dentistry, the most common use of the adjective “anterior” is in conjunction with the word “teeth” to identify a group of front teeth named the anterior teeth. Dentistry commonly thinks of the anterior teeth as the upper and lower canines, laterals and centrals, which may be presented in any combination of teeth, crowns, partials, implants, or space. Dentistry uses the word “anterior” as a slang term for the space from canine to canine on the upper and lower arches. However, when talking about occlusion, the word “anterior” means “in front of the condyles.”
The word “guidance” is defined in the Oxford dictionary as “the process of guiding or being guided.” Guidance, in dental occlusion, is defined in two ways: “What process is being guided?” and “What process is doing the guiding?” The process that is being guided is the mandible. The mandible is one bone and includes the condyles, lower arch and the mandibular teeth and it is being guided into the upper arch for occlusal function. The million-dollar question in the study of occlusion is: “What process is doing the guiding?” The answer to this question is the best-kept secret in dentistry because it can change over time.
The anatomical structures, such as TM joints, muscles, ligaments, and teeth, direct the mandible into the maxillary arch. If all of the anatomical structures are in harmony and independent of each other, then guidance is efficient and the anatomy will protect itself. Dysfunction begins when form and function are not in harmony and the anatomy must work against itself.
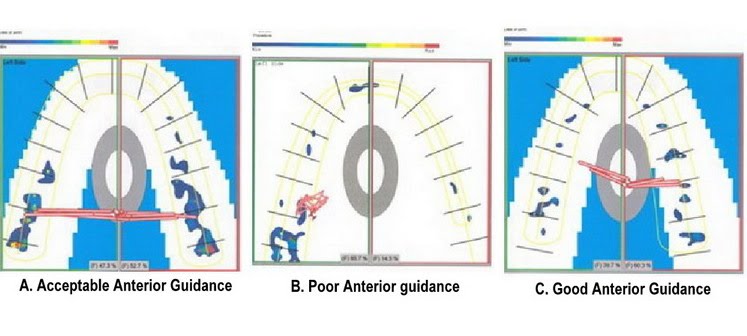
Every occlusion has its own distinctive characteristics and controls that give the anterior guidance its signature pattern. Occlusion (“occlude” means come together) is “Anterior Guidance,” and is defined as the sequence of any tooth that touches first, second, third, etc., until the maximum number of teeth are squeezed together. Anterior Guidance (Occlusion) is a pattern of closure contacts that repeat itself every time teeth come together. When patients tap their teeth into a T-scan computer sensor (i.e. digitized articulating paper), a pattern of force shows a repeating map of closure contacts. These patterns are displayed in a 3-D movie of the patients’ occlusion and/or their anterior guidance. The three T-scan patterns below show three different anterior guidance patterns. The first pattern (scan A) is an example of acceptable anterior guidance because the right and left arches are similar. The second (scan B) is an example of poor anterior guidance because the posterior left teeth are trapped against the lateral pole of the left condyle. Finally, the third pattern (scan C) indicates good anterior guidance because the canines are very close to immediate disclusion in any movement.
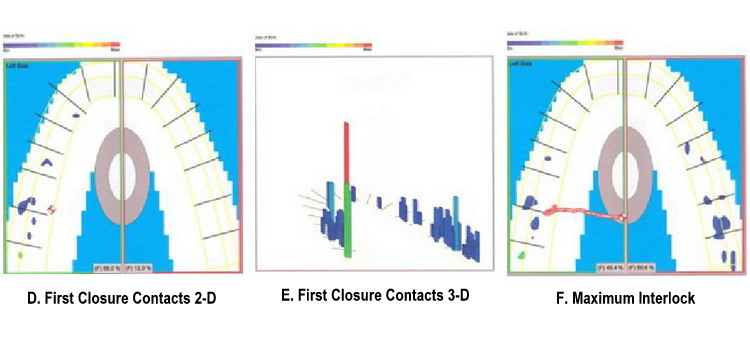
The first tooth that touches is called the “anterior control.” There always is an anterior control in occlusion! The first contact may either be adequate or inadequate. The anterior control is the beginning of the series of contacts that guide the mandibular teeth into the upper occlusal plane. The anterior control is the beginning of the anterior guidance and the beginning of the occlusion. In general, if a posterior molar is the first tooth to touch in centric closure, then the patient probably has an adaptive anterior guidance. Canines and bicuspids that touch first generally indicate a favorable anterior guidance. It may be difficult to understand that a posterior tooth controls the anterior guidance in most occlusions. As stated before, the adjective “anterior” in “anterior guidance” means “in front of the condyles” and does not mean the front anterior teeth. A pathologic occlusion almost always has a posterior tooth controlling the anterior guidance, as shown in the next set of T-scans. The anterior control (tooth #15 against tooth #18) is directing the mandibular closure in a lateral direction to the right until the occlusion locks. Scan D is a 2-D frame showing the first closure contacts. Scan E is a 3-D picture frame illustrating the anterior controls as the bite closes. Scan F is a 2-D frame of the teeth in maximum interlock.
In a young, healthy occlusion, the teeth do most of the guidance work. If the triad of teeth, muscles, and joints are able to function independently of each other, the occlusion will be stable for decades. However, in a pathologic occlusion, the three elements of the triad are dependent on each other and the powerful muscle engrams accelerate the aging of the teeth and TM joints. The teeth (posterior and anterior) and their position in the arch are responsible for ‘teaching’ the habitual muscle sequence required to chew and function. At age 10, the remaining primary teeth are flat and worn, and one of the first molars is the anterior control. As the adult posterior teeth and canines erupt, a second molar or a first bicuspid is the most common tooth to touch first in centric closure at age 14. In a young adult (age 20-40), the sequence of teeth touching becomes critical when defining good anterior guidance and bad anterior guidance. As we go through life, our centric position changes because one condyle will age at a different rate than the other. As centric relation changes, our anterior guidance and envelope of function change as well. Slow change is called “adaptation” and accelerated change is called a “pathologic occlusion.”
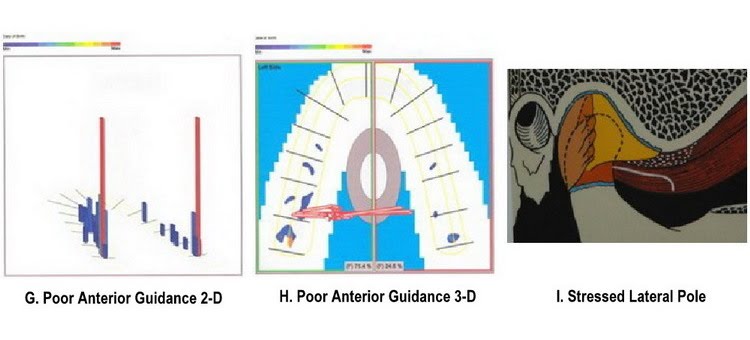
The analogy that I like to use with our patients to describe how the posterior teeth should fit together is similar to closing a perfectly balanced door. When the mandible closes, the two healthy TM joints (the hinges) rotate the lower posterior teeth (the door) to stop and fit perfectly into the upper posterior teeth (the frame). In this position, all the posterior teeth should stop with equal, simultaneous contact in one single plane. A perfectly true closure involving up to 32 teeth coming into equal stops in exactly one plane favors theory more than reality. A lot of puzzle pieces have to fit perfectly in order for any system to function cleanly every time. If a door closes poorly, drags on the floor, or wedges into the frame before closure, then the system functions poorly. The door is able to close but the space between the door and the doorframe is not symmetrical. The question now becomes: “Is it the door, the hinges, the door frame, or all three that are out of alignment?” Healthy condyles in a good, braced, centric position are similar to tight door hinges. Pathologic TM joints lead to poor anterior guidance and eventually the door and the doorframe continue to force each other further out of alignment. The 2nd molar anterior control in the T-scan below is a good example of a patient with a jaw disorder and a poor anterior guidance. Scan G (3-D format) and scan H (2-D format) are both the same images. In this patient, both condyles are stressed at the lateral pole and not able to find centric, as shown in Illustration I.
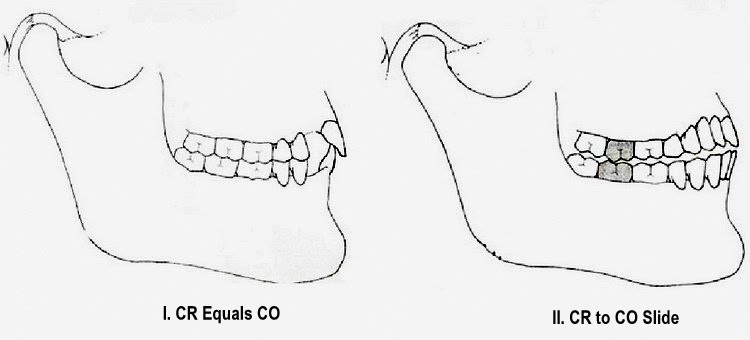
CR Relationship to CO
Picture I (occlusion is close to CRO) and Picture II (posterior interference, CRO is not possible)
Dr. Hollenbeck states that a good occlusion has two major components. The first condition is a “good centric” (i.e. strong tight hinges) defined in the previous article What is Centric and the second condition is “no interferences.” To help define the concept of “no interferences” in dentistry, I will refer to two master teachers in dental occlusion. The first is Dr. Skyler, famous for the Pankey, Mann, Skyler Occlusal Concepts taught in most dental schools. Dr. Clyde Skyler said: “In the occlusal rehabilitation of a natural dentition, there are three factors which have an influence upon, or establish the occlusal contours of the posterior teeth. They are the two posterior controls, or the temporo-mandibular joints, and the anterior control.
These three controls function to a degree separately and independently, but if there is to be efficiency and harmony of functional occlusion, all intermediate contours of the teeth will be influenced by them and must function in harmony with them.” Dr. Peter Dawson explains the concept in a similar way in his textbook Evaluation, Diagnosis, and Treatment of Occlusal Problems by stating: “The occlusal contours of all the posterior teeth are dictated by both condylar guidance and anterior guidance. No posterior tooth should interfere with either anterior guidance or condylar guidance. Posterior teeth may either be discluded from any lateral contact by the anterior teeth, or they must be in perfect harmonious group function with them and the condyles.”
The combination of the two statements that Dr. Hollenbeck makes (good centric and no interferences) is the foundation for teaching occlusion. As soon as condylar guidance, anterior guidance and incisal guidance become dependent on each other, an occlusion will show signs of stress. Stress signs start out subtly: an asymptomatic click in the TM joint, craze lines on the enamel of the teeth, abfractions, or soft tissue irregularities in the periodontium.
The ligaments holding the TM joints and the ligaments supporting the teeth become dependent on each other and adapt or age quickly. Muscle patterns and the envelope of function change as the joints, teeth and periodontal foundation function against each other. Change can be physiologic (i.e. natural aging) if the condyle guidance, the anterior guidance and the incisal guidance slowly adapt together over decades. However, change is pathologic if the guidance systems are strongly dependent on each other. Understanding the relationship between the condyles (i.e. “a good centric”) and the teeth (i.e. “a good anterior guidance”) is unique to each occlusion and will take every dentist a lifetime to try and master.
The concept of anterior guidance and posterior teeth has a second phrase that is often overlooked in function. The dominant theme of this concept is the definition of how the teeth come together. The second half of the question is: “How do they come apart?” What happens when the teeth come to a complete stop and reverse direction? The question may seem simple, but the answer is not to be found in any text book or in any article in my library. You will find our attempt at answering this question in the concept Incisal Guidance and Anterior Teeth.