
The idea that a tooth can develop a non-carious lesion is not a new concept for dentists. Teeth age from young to old and they change internally and externally throughout a lifetime (see photo A and B). Dentists understand receding pulps, affected dentin, enamel craze lines and wear facets. However, dentists differ about the etiology as a tooth changes shape at the CEJ over time.
A
C
B
D
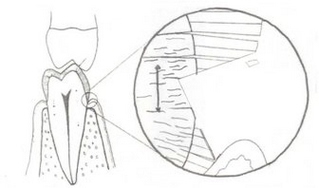
G.V. Black (the “father” of modern dentistry) details the concept of how teeth change in his “bible” of operative dentistry. The first volume, titled “Pathology of the Hard Tissues of the Teeth,” describes how the German dentists in the late 1800’s wrote about wedge shaped areas of erosion named keilformige defecte (see photo C and D). Dr. Black in the second edition in 1914 described the non-carious cervical changes we see as teeth age.
“These are the keilformige defecte of German writers. This form usually has its place of beginning near the free margin of the gum, and if seen at its beginning looks like a little groove cut across the crown of the tooth from mesial to distal. These gradually deepen, and soon the case looks as if a wedge-shaped piece had been cut out of the labial surface of the tooth, presenting a flat side reaching toward the gingival and a square shoulder toward the occlusial, as if filed away with a square file. In many of the cases, the cut is as square and the angles as sharp as they could be made with such an instrument. In others there is more inclination to rounding of the angle in the deeper part of the cut.”
G.V. Black included keilformige defecte in the same category as erosion. Two of the eight possible etiologies Dr. Black gave for erosion were:
Erosion is the result of the action of an acid in some way, as yet unknown to us.
Erosion is caused by friction, most generally of the toothbrush carrying same abrasive tooth powder.
In 1907 a Dr. W.D. Miller of Germany published his results of a two year study on the etiology of erosion. He mechanically brushed teeth with different acids and tooth powders trying to create a cervical lesion. Dr. Black said of his work, “I saw none of his artificial production of the sharp, clean-cut margins so often present in the mouth. I am not yet convinced that all erosions are produced in this way.”
A century later, dentists have a new word for keilformige defecte named “abfractions”. Today, dentists (about 50%-78%, depending on the study) still believe abfractions are a form of toothbrush abrasion. It is possible that a toothbrush is a variable in the abfraction equation; however, teeth are biologic tissue, with multiple functions, and are subject to many different environments over their lifetime. This article explores the different etiology’s the profession currently believes about abfractions.
The modern day etiology of abfractions comes from many dentists. Dr. Gene McCoy and Dr. John Grippo are two pioneers who advanced the idea that repetitive micro-trauma over time will change the shape of a tooth. In the early 1990’s, Dr. Grippo introduced the term “abfraction” (from the Latin words ab – “away” plus fracito – “breaking”). He describes how the hydroxy-appitate crystals of the teeth fracture and break away or “abfract” from the tooth. “Abfraction,” as a sub-set, is one of the many non-carious pathologic and physiologic changes occurring in a tooth over its lifetime. A non-carious lesion is defined as a loss of tooth substance caused by something other than trauma, caries or developmental defects. Additional sub-sets of non-carious lesions are attrition, abrasion and erosion. Dr. Grippo defines the four classifications of hard tissue lesions.
Attrition – the physiologic wearing away of tooth substance as a result of tooth-to-tooth contact, as in mastication. Attrition is most noticeable on occlusal and incisal surfaces. It may also occur at the interproximal contact points as result of the anterior component of force, where small horizontal and vertical movements of teeth occur during function, thus causing frictional wear. The overall effect of this physiologic wear is a reduction of 0.5 cm in length of the dental arch from the third molars to the midline by the age of 40 years. Attrition involves biomechanical principles and is physiologic.
Abrasion – pathologic wear of tooth substance through (abnormal) biomechanical frictional processes, either extrinsic or intrinsic. Extrinsic examples are improper or excessive tooth brushing (mainly affecting root surfaces) and noxious oral habits such as biting a pipe stem, biting fingernails, holding pins between the teeth, etc. Bruxism is the most destructive intrinsic manifestation of abrasion. (See Photo H)
Erosion – chemically induced loss of tooth substance, mainly through acid dissolution. Erosive acids may have an extrinsic or intrinsic origin: the former through diet; e.g., citrus fruits or juices, carbonated soft drinks, baby bottle syndrome, or air (in some industrial chemical plants): the latter through regurgitation of gastric acids, due to vomiting as seen in bulimia, pregnancy morning sickness, or hiatal hernia. Acid reflux is the most common form and is increasing with each generation because it is associated with obesity.
Abfraction – pathologic loss of hard tissue tooth substance caused by biomechanical loading forces. These lesions are due to flexure and ultimate fatigue of enamel and dentin at a location away from the point of loading.
In 1984, Lee and Eakles describe the tensile strain on the cervical neck of the tooth. They developed the diagrams below as a theory to show how a tooth will change when a loading force is not directed along the long axis of the tooth. (See E and F).

E
F

G

H
The longevity of dentate humans continues to improve with each generation increasing the duration of force a tooth must resist over a lifetime. Every tooth is unique in growth, development and service throughout its lifetime. Each abfraction is unique in form, angle, depth and each tooth receives different direction, frequency, duration, location and intensity of force. To date Dr. Grippo has defined 15 different styles of abfractions: five in enamel and ten in dentin.
Types of abfractions
- Enamel- hairline cracks, striations, saucer-shaped, semilunar-shaped, cusp tip invagination.
- Dentin- Gingival, circumferential, multiple, sub-gingival, lingual, Interproximal, alternate, angular, crown margin, restoration margin.
Abfractions have multiple combinations of the 15 styles. This is because the enamel takes the direct force and the CEJ of the tooth takes the tensile force generated from the direct contact. As cusp tips implode and enamel craze lines deepen, the biologic tooth must try to defend itself. The heal of your foot is the best example of a surface skin change as you use or abuse your feet. Teeth scar, adapt and evolve as they age in their own individual way, under their own unique circumstances. Attrition, abrasion and erosion generally weaken the structure of a tooth and encourage the abfraction to develop as the compressive and tensile forces add up over time.
Photo G can be classified as severe attrition if the diagnosis is physiologic wear. Or, it can be a combination of attrition, abrasion and cusp-tip abfraction if the diagnosis is both physiologic and pathologic. Photo H is a patient who has a lifetime history of bruxism; so the non-carious lesions may be classified as severe abrasion or a combination of advanced attrition, abrasion, erosion and many styles of abfraction.

I

J
Abfractions have an incredible number of variables that produce the myriad shapes, size and characteristics of each. The heredity composition of the dentin, enamel and the bond strength of the hydroxy appitate crystal structures within the tooth, may be the most important factor that predisposes a tooth to an abfraction. Other factors include the size, shape and anatomical characteristics of each individual tooth. For example, does the individual tooth have a large coronal segment and a small root support or vice versa? The position of the tooth within the type of occlusion scheme (class I, II, III) often dictates the force the tooth receives. (See photos I &J) In addition, some teeth are tilted, twisted, or turned either alone or in combination with the entire arch. The location, frequency, duration and intensity of tooth contact are all contributing factors to the style and characteristics of the abfraction. The number of variables that predispose a tooth to an abfraction are many. The infinite number of combinations of variables makes for a challenging diagnosis. Photo I is interesting because the lower canine (#27) hits the upper central (#8) in left lateral movement, producing a vertical style abfraction. In photo T the teeth favor a class I occlusion, but the bone relationship favors class III.
The position of the tooth within the alveolar foundation and the strength of the alveolar bone are very important etiologic factors. The health of the tooth’s foundation support system can play a strong role. For example, the periodontal support may be susceptible or resistant to bacterial disease. Bone that is resistant to bacteria is stronger and less likely to form periodontal pockets. If the root is anchored into the bone, then the CEJ will flex more than a tooth in porous bone. Many teeth present cervical adaptation, in addition to bone loss, recession, and pockets. The bone in this patient is rock solid, but the excessive force on only the nonworking cusp finally torqued the tooth out of its socket.

K

L
Photo M shows the upper first bicuspid before the tooth was extracted. Bone loss and a periodontal abscess eventually lead to the extraction. The abfraction took decades to develop. The position of the tooth in the arch and the function of the tooth are strong factors in abfraction etiology. Tall teeth with long roots and only cusp tip function, tend to flex more than flat teeth with multiple contact points. The photos K and L show a rare example of a classic abfraction without attrition, abrasion and/or erosion as a strong predisposing factor. The only wear facet in photo L is the buccal cusp tip of tooth #12. In photo K the non-working cusp had a stressful position in the arch and the tensile stress on tooth #12 increased when #15 was extracted and #13 fractured years previous.
Dr. McCoy describes engineering principles to show how hard tissues fatigue and compress due to tensile and compressive loading forces. He talks about the sheen or polished glassy appearance characteristic to abfractions. The explanation is that both the teeth and the bone are composed of collagen and when collagen is compressed, electricity is produced. Positive ions are emitted through focal points of high stress resulting in the polished effect. The cervical notch in photo L is a beautiful example of the polished glass-like tooth structure with-in the abfraction.
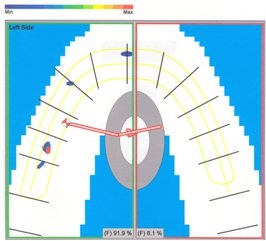
The photos M and N show an upper first molar (#14) with recession, wear facets, attrition and a notched abfraction on the MB root. The two T-scan prints (O and P) illustrate the force this tooth receives every time it touches #19. As a patient taps into a force sensor, scan O shows how the force travels across the occlusal table from right to left. Scan P is a 3-D print that illustrates the intensity of force onto the MB cusp of #14.

M

N
O

P
Teeth are living tissue and abfractions can be active or passive. Active abfractions are similar to a small paper cut on the outer surface of the skin. The tooth heals the open surface wound and scars it over until the next micro-fracture or paper cut occurs. This process may continue for a number of years until the tooth conforms and scars. An active abfraction can accelerate the tooth from a physiologic adaptation to a pathologic problem. Active abfractions produce sensitive teeth that can be a diagnostic and a clinical problem for any dentist regardless of specialty. Photo Q is a very painful abfraction.

Q

R

S
T
The abfraction in photo Q is an active abfraction, while the abfraction in photo R is not. In photo Q, this new patient presented with a painful cervical abfraction on #5, which started when the lower crowns were placed two years pervious. The only wear facet on tooth #5 is the buccal cusp tip similar to the tooth in picture K. The etiology of this lesion mostly favors abfraction and minimal attrition, abrasion or erosion.
Some abfractions scar and change shape without any sensitivity and the teeth seem to compress and get stronger around the CEJ of the tooth. Many of these teeth do not have sharp notches but are flatter or disc-shaped and appear compressed. Teeth under compressive forces tend to flatten at the CEJ, while teeth under tensile forces tend to notch at the CEJ.
Photo R shows another upper first bicuspid in a 30-year-old female. The upper primary canine is still present because the adult canine is impacted. Primary teeth can abfract like an adult tooth, but usually fracture when retained for many years.
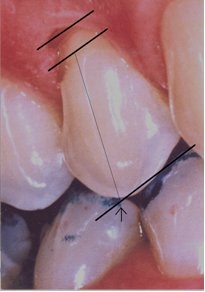
Virtually, all cervical abfractions have an enamel craze line at 90 degrees to the angel of the abfraction, and the force plane generated across the tooth. The arrow in photo T points to the contact point that generated the enamel crack. The plane of force across the non-working cusp is parallel to the angel of the notch as demonstrated by the thick parallel lines.
Mother nature has blessed us with the most biomechanical perfect system evolution can design and we, the people, have found every possible way to stress the stangthnomathic system. Missing teeth, bridgework, crowns, attrition, abrasion, erosion, and stress adds up over the years. Engineering principles teach us that force has to be diverted or absorbed and that is exactly what happens when you occlude. Occlusion means come together and when teeth touch either in function or para function, a force is generated. Excellent occlusions do a better job at diverting force. Force directed along the long axis of the teeth on working cusps rarely abfract. Stressed occlusions tend to absorb force. Teeth that absorb force on non-working cusps and not along the long axis of the teeth have a greater incidence of abfractions and other pathology such as wear facets, broken cusps, recession, bone loss etc. Abfractions, wear facets and enamel cracks teach us how stress is being transferred across the teeth and the occlusal table. Abfractions are really an advanced stage of attrition, abrasion and erosion or a combination of all of the above. The combinations of non-carious lesions describe a history of how the occlusion adapts and ages over time. The anatomical change with-in and around a tooth over many years has a history and is a diagnostic indication that should be considered.
Abfraction is a subset of non-carious loss of tooth structure. Teeth are living tissue and are supported by ligaments that fatigue and compress over time. When a tooth looses its shock absorbent effect and is stressed into the alveor bone, a functional or dysfunctional force is applied over time. Some patients loose bone, but dentistry is saving teeth and eliminating periodontal disease, making it possible for more teeth to abfract. Abfractive lesions are caused by flexure and ultimate fatigue of susceptible teeth at locations away from the point of loading. The clinical patient presents with myriad combinations in a variety of enamel and dentin lesions. Non-carious lesions are a wonderful history of diagnostic information that detail how force in the occlusion has affected each tooth.
The angle and position of the abfractions make the theory of toothbrush abrasion difficult to understand because the angle of the lesion is not horizontal like a toothbrush stroke. The etiology of keilformige defecte has taken 100 years to develop and it might be possible that it will take another century before we fully understand the true diagnosis of abfractions.
In 1994, Dr’s Lambert and Lindenmuth provided an excellent literature review of abfractions and the conclusion stated:
“Evidence presented by the relatively new science of bioengineering seems to confirm …that tensile stress resulting from occlusal forces is the primary cause of cervical erosion. The new term “abfraction”… is beginning to be recognized and accepted by the profession and will…soon be a common diagnostic entity.”
